Gestational Diabetes is a type of glucose intolerance or diabetes that develops in pregnancy.GD usually appears in the middle of pregnancy between 24-28 weeks.
The prevalence of GD is 10 % worldwide and it is around 15 % in India. This could be attributed to the poor nutritional status overall.
Physiological insulin resistance occurs both in puberty as well as pregnancy. In Nature, Nothing really happens without a reason. Both the stages are associated with growth spurt. We all know that insulin is an anabolic hormone and the compensatory increase in insulin levels (compensatory hyperinsulinemia) help the foetus to grow at a rapid pace which is actually required during pregnancy.
Your healthcare provider will test your blood sugar during pregnancy. The test may have two parts viz., 1. Glucose Challenge test – using a sweet liquid. After an hour, you will have a blood test to check your blood sugar level. 2.Glucose Tolerance Test if your challenge test results are unusual. GD screening is routinely done between 24-28 weeks of gestation. At this stage, hormones start getting produced by the placenta. This organ forms in the uterus and supplies the fetus with oxygen and nutrients. The hormones it makes can interfere with insulin. However, the screening is done early for at-risk pregnancy in which there is prior history of GD/PCOS/ Obesity/ Known glucose Intolerance/ BMI>25 to prevent the complications associated with hyperglycemia to both mother and the fetus.
GD usually don’t produce any symptoms and that’s the tricky part. But some people experience frequent urination, nausea, thirst and tiredness. There are usually no warning signs of gestational diabetes. Symptoms are mild and often goes unnoticed until you are tested for diabetes in the second trimester of pregnancy.
If uncontrolled , it may lead to complications such as macrosomia in baby, premature delivery, respiratory distress syndrome in infants, hypoglycemia in the baby, risk of future diabetes in the baby as well as the mother, high blood pressure and Pre-eclampsia in mother.
If you are diagnosed with gestational diabetes, nutritional recommendations based on calorie model is done. Avoiding junk foods, processed foods and sugary drinks. Eating smaller meals more often. Exercise often plays an important role in glycemic control. You can talk to your healthcare provider about creating a safe exercise plan, tailored to your unique needs in terms of age, fitness level before pregnancy, overall health and weight. People with diabetes typically have more prenatal visits to check fetal growth (via ultrasound), monitoring of weight gain and discussion with the healthcare provider.
Compensatory hyperinsulinemia due to physiological insulin resistance occurs in pregnancy. It is partially mediated by HTR2B receptors (serotonin receptors) for beta cell proliferation. Serotonin synthesis is dependent on vitamin B6. Low B6 causes failure of beta cell proliferation that contributes to the development of GD.
Interestingly around 40% of women are B6 deficient during pregnancy.
There is a knowledge gap between the scientific researches and the current clinical practices. Much of the scientific researches often go in vain even it contributed some valuable information to the scientific communities. The scientific researches (most of them being funded by the tax payers money) are not actually translated into clinical practice at a desirable pace for the welfare of the population. It is influenced by the Big Pharma and Food industry in the regulation of guidelines and protocols. One such example is the neglect of the importance of vit B6 with relevance to Gestational Diabetes.
Nearly 50 years back, the relevance of vit B6 in GD was published in a world’s renowned scientific journal, BMJ under the title – Improvement of Oral Glucose Tolerance In Gestational Diabetes by Pyridoxine (July, 1975).
During gestation, there is an imbalance in the Trytophan-Nicotinic acid metabolism and needs more of the rate-limiting coenzyme Pyridoxal 5’ Phosphate. Consequently, nearly every pregnant woman will develop a relative pyridoxine deficiency as shown by an increased urinary excretion of tryptophan metabolites, particularly xanthurenic acid, after oral administration of L-tryptophan.
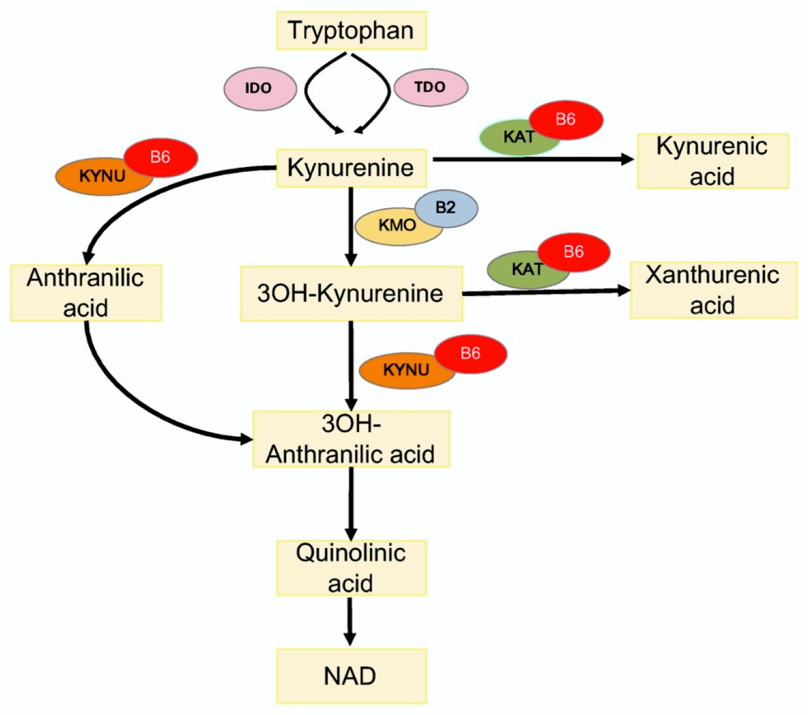
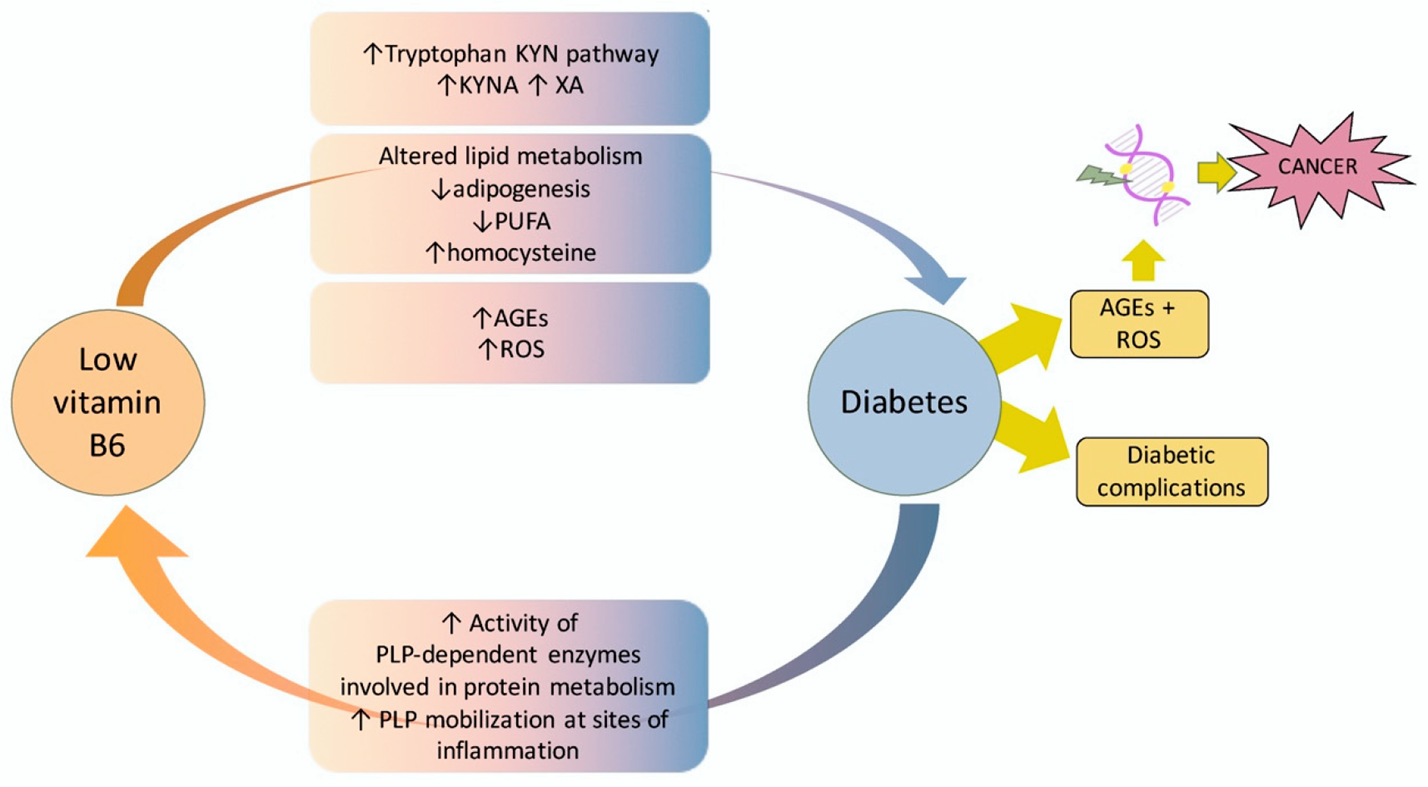
Relative Pyridoxine deficiency leads to the production of Xanthurenic acid (a tryptophan metabolite). Xanthurenic acid is an insulin antagonist thereby inhibiting its functions. Hence increased Xanthurenic acid in relative vitamin B6 deficiency leads to impaired glucose tolerance. Supplementation of vitamin B6, 100 mg daily for 2 weeks reduces the xanthurenic acid to normal levels and it significantly improved glucose tolerance, curing GD in most of the cases. In this particular study, patients responded very well to another course of vit B6 supplementation if they were poor responders initially.
It's totally disheartening to see so many of the pregnant women developing gestational diabetes. Adding more fuel to the fire is the total lack of concern in the last 50 years for overlooking such valuable research and not being translated into clinical guidelines and protocols. Our centers’ experience with the supplementation of vitamin B6 in GD is extremely encouraging, eliminating the need for insulin and avoiding the complications associated with gestational diabetes. Every woman with gestational diabetes or even with the risk of GD should be supplemented with Vitamin B6 100 mg once daily or 40 mg thrice daily for 2 weeks. I hope this implementation comes into clinical practice of every obstetrician and gestational diabetes should no longer be a nightmare anymore !!!