The common myth among the people and even most healthcare professionals is that management of diabetes is all about blood sugar numbers by medications. This symptomatic management is usually done by modulating the number of drugs, its dosage, titrating it every month or even adding insulin if there is poor response to the drugs. Elevated blood sugar is just a sign of the underlying condition called insulin resistance. Perhaps diabetes is a very late manifestation of insulin resistance that is often neglected in the first place. Treating the blood sugar with insulin or insulin secretagogues without reducing insulin resistance actually accelerates the disease process and the patient may develop complications earlier particularly, cardiovascular complications like heart attacks, strokes and peripheral artery diseases.
Diabetes is diagnosed by elevated blood glucose levels. The blood sugar level goes up only when the high insulin levels (a compensatory response) is no longer able to compensate for the underlying insulin resistance. Insulin resistance and elevated insulin levels (hyperinsulinemia) are two sides of the same coin. Early spectrum of insulin resistance is characterized by normal glucose levels and high insulin levels. This early spectrum is most often asymptomatic, and it spans over a period of 5-15 years, before a person becomes diabetic. The diagnosis of pre-diabetes or diabetes is usually made in a very late stage, since it manifests only in the late spectrum of insulin resistance when the elevated insulin is no longer able to compensate for the underlying insulin resistance (decompensated) and the glucose levels starts raising now. Interestingly, the complications of diabetes particularly the macrovascular complications start to develop, even before the diagnosis of diabetes due to the insulin toxicity (long term exposure to high levels of insulin).
Normally, in a healthy insulin sensitive person, both the blood glucose & the insulin levels are within normal limits. When a person starts developing insulin resistance, at least in the initial 5-15 years the patient has high insulin levels (elevated even up to 3-7 times the normal limits) as a compensatory response by secreting more insulin from beta cells of pancreas. This compensatory response actually depends up on the insulin reserve. At this stage, the blood glucose levels are absolutely normal. We are highly misled by the glucose numbers because we often correlate metabolic health or insulin sensitivity with glucose levels. Normal glycemic status does not reflect the true nature of metabolic health.
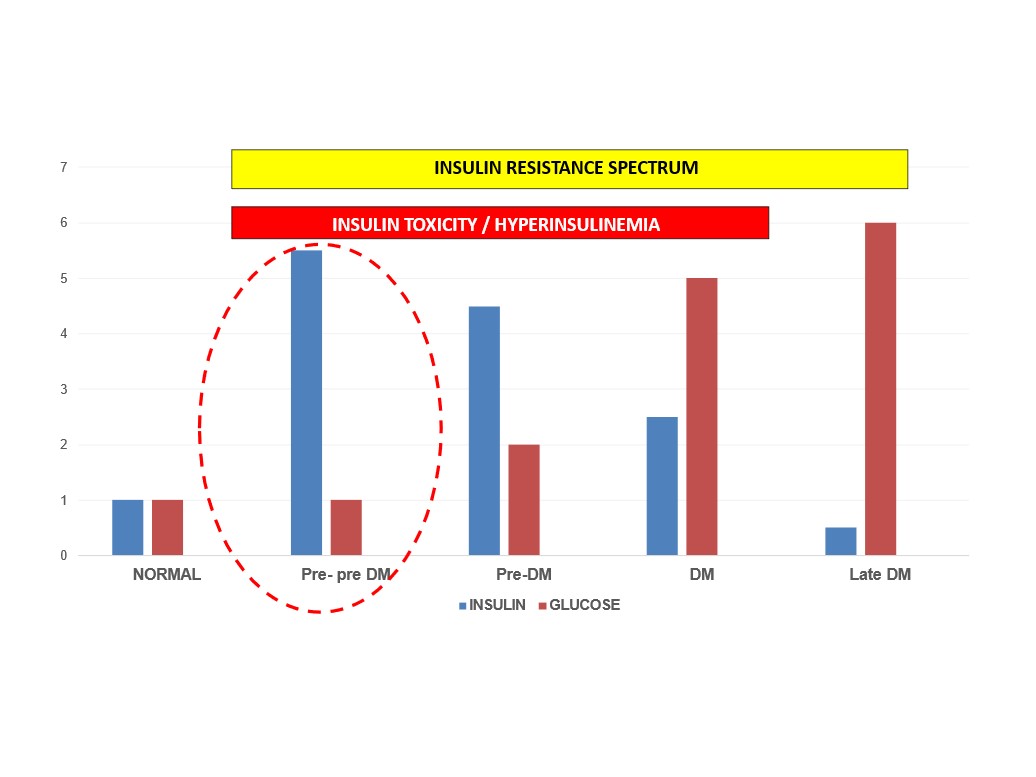
Even annual health checkups or master health checkups fail to take fasting insulin levels (a measure of insulin resistance) and the medical fraternity is focused only on the total cholesterol levels and the LDL-Cholesterol in the lipid profile & if found elevated, there is a tendency towards reflexive prescription of statins (cholesterol lowering drugs) and low-fat diet recommendations. The atherogenic dyslipidemia (elevated triglycerides and reduced HDL-Cholesterol) which is actually a measure of ectopic fat from the liver is often ignored and neglected. What we have to worry is actually ‘Dyslipidemia’ and not the total or LDL-Cholesterol, because it carries a greater risk for heart disease, as per the recent scientific research studies. Dyslipidemia is a ‘silent scream’ from the liver. It is a surrogate marker of insulin resistance. Unfortunately, the early spectrum of insulin resistance remains asymptomatic for several years before manifesting in terms of metabolic dysfunctions. If we are able to diagnose insulin resistance by simply looking at the fasting insulin (> 6 mU/L) or the triglyceride-HDL ratio (TG:HDL-C >1.3), it is possible to prevent every single case of type 2 diabetes from manifesting in the first place. Isn’t it really fascinating?
“No person in the world deserves type 2 diabetes because we as healthcare professionals (when empowered with adequate knowledge) can prevent diabetes from manifesting in the first place by nearly 100%”
Our literature is greatly influenced by the west. The dietary protocols are not an exception. The West blame the carbs as the reason for metabolic syndrome, especially diabetes. To be honest, The West has no idea about the Traditional Indian diet, variety of grains, pulses, lentils and beans. Moreover, the spices we use in our diet are rich in micronutrients, aids in digestion, assimilation as well as in metabolism. For example, black pepper (rich in Vanadium) aids in carbohydrate metabolism, ginger in protein metabolism and long-pepper in fat metabolism. Well-formulated high fiber diet with complex carbs, moderate proteins and healthy fats is as good as Ketogenic diet. Tropical climatic conditions throughout the world favors agriculture throughout the year, since we have a constant supply of food throughout the year which can be easily stored for several months, our cuisine is based on complex carbs. The very reason why the people in the East, especially south Asian including Indians have less Personal Fat Threshold (PFT) as compared to the west. We don’t to store large amount of fat to face adversity over thousands of years because of the favorable climatic conditions and prosperous soil. Whereas the Western countries, in the temperate regions have mostly cold climate with good sunlight exposure limited only to 3-4 months in a year, which necessitates increased storage of energy in the form of fat, primarily for survival (increased PFT). The West except in the last 100-150 years, till industrialization and globalization were highly dependent on animal-based diet for thousands of years. This is the very reason why the people in the west have higher Personal Fat Threshold, even though they may be overweight and obese, metabolic complications starts at a later date comparatively. This could be compared the same story of Goat (lean) vs Sheep (fat) in terms of adaptation to climatic conditions with different body composition. Embracing cultural habits in formulating diet is an art to be learnt and practiced in clinical practice.
Healthcare professionals are treating diabetes as if the blood glucose is the only problem (Glucose-centric paradigm). Hence, they often fail to address the underlying insulin resistance. The sensible way to treat diabetes is to reduce insulin resistance and normalize it if possible. Blood glucose numbers are just a reflection of insulin resistance. If the insulin resistance is reversed, then diabetes can be kept in remission lifelong.
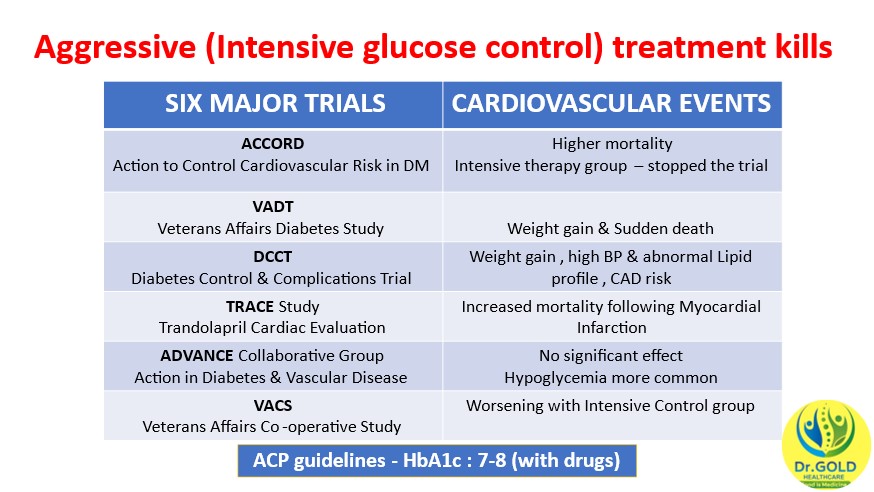
History repeats if we fail to learn!! Conventionally, it was thought that if we are able to control glucose levels with medications or insulin, the complications can be reduced drastically. Surprisingly all the six major trials clearly suggested that intensive glucose control with insulin or drugs often resulted in increased cardiovascular events and mortality. This is not a paradoxical response because the intensive groups were given more insulin and insulin secretagogues for strict glycemic control, but it actually increased the insulin toxicity. It is worthwhile to remember that fasting insulin (Insulin Resistance) is the most important predictor of heart disease. Hence, ACP guidelines recommend achieving the target of HbA1c of 7-8 rather than intensive control (6-6.5) when treated with drugs. However, it should be noted that strict glycemic control is encouraged when the patient is treated with lifestyle modifications rather than drugs.
The optimal approach to type 2 diabetes is to reduce the insulin levels or in other words, the insulin resistance. Lifestyle modifications (Diet rich in Proteins, healthy fats along with micronutrients and fibers) focusing on the body composition is of utmost importance and should always be the first line in the management of diabetes. Drugs such as Metformin, SGLT-2 inhibitors and GLP-1 analogues have better cardiometabolic profiles compared to other drugs but there are not without side effects. Insulin should be given only for acute glycemic control in times of stress like medical emergencies or surgical for short term. Routine prescription of Insulin, Insulin secretagogues like sulfonylureas and meglitinides actually increase the already existing insulin toxicity. These drugs can be selectively used in minimal dose, in patients with advanced cases of diabetes with insulinopenic response for achieving optimal glucose levels. The whole population should be sensitized enough about the possibility of achieving higher rates of remission in the initial years and the patients should be encouraged to achieve and maintain remission as soon as the diagnosis of type 2 diabetes is made. However regular and frequent follow-ups are necessary even after achieving remission to prevent re-reversal of diabetes. Generally, for type 2 Diabetes particularly in the early stage, “Reversal is the rule rather than exception.”